EXTOD Healthcare Professionals South Conference: delivered by EXTOD and organised by SBK Events.
This unique forum was created to equip Diabetologists, Diabetes Specialist Nurses, Dietitians and Paediatricians with the knowledge, inspiration and practical understanding to support type 1 patients to undertake safe and effective exercise.
Please click on the EXTOD courses tab for details of further courses available.
Evidence-based presentations, case study led workshops and invaluable lived experience
This EXTOD day provided attendees with current, evidence-based knowledge on managing Type 1 diabetes for exercise. Those who joined were able to speak with experts in the field and left with practical advice and clear strategies to use with patients with T1D in a clinical setting.
EXTOD Healthcare Professionals South Conference featured case study led presentations on:
- The challenges someone with Type 1 diabetes faces when exercising
- The elite female athlete
- Exercise setting for each pump / closed loop system and how to use these settings for exercise
Plus discussion driven workshops on:
- Assessment and starting advice for exercise
- Basic insulin changes to improve glucose control around exercise
- Special circumstances: Low carb diets, hot and cold weather adaptations
- Getting the most out of a continuous glucose monitor when exercising
- Using dietary intake to improve glucose control around exercise
- Using exercise to control glucose around exercise
- Managing race /event day: what to do prior, on the day and postrace management
- Dealing with multisports and how to plan changes
With thanks to JDRF and DRWF for supporting this educational conference:
| 8:30 |
Registration and refreshments
|
| 9:00 |
Welcome
Prof Parth Narendran, Diabetes Research Unit and the Type 1 Diabetes Clinical Service Lead, University of Birmingham and The Queen Elizabeth Hospital
|
| 9:10 |
The challenges someone with Type 1 diabetes faces when exercising
Dr Matt Cocks, Exercise Physiology Lecturer, Liverpool John Moores University will discuss the following therapies: exercise, diet, finger and continuous glucose monitors, insulin, insulin pumps and closed loop systems
|
| 9:50 |
Diabetes management insight: athletes completing the coast to coast in a day ride
Wendy Frost, Lead Dietitian, Wessex Children and Young People’s Diabetes Network and Leader of Team Type One Style and Henry Aspden, Leader, Team Type One Style
|
| 10:30 |
Networking break
|
| 10:50 |
Workshops 1a – 1e
These workshops will be run twice in the morning.
|
| Choose your first morning workshop from the following: | |
|
1a - Assessment and starting advice for exercise
Prof Parth Narendran, Diabetes Research Unit and the Type 1 Diabetes Clinical Service Lead, University of Birmingham and The Queen Elizabeth Hospital and Barbara Hudson, Clinical Nurse Specialist in Diabetes, University Hospital Birmingham NHS Foundation Trust will discuss the following therapies: history taking, complications, injections sites, insulins, glucose monitors, glucose targets
|
|
|
1b - Basic insulin changes to improve glucose control around exercise
Claire Foster, Diabetes Dietitian and Giorgio Carrieri, Lead Nurse, Children's Diabetes Team, Somerset NHS Foundation Trust will cover: insulin, insulin pumps and closed loop systems.
|
|
|
*Recommended for first time attendees*
If this is your first time attending EXTOD day then we would suggest picking the above workshops as these will give you a good grounding.
|
|
|
1c - Special circumstances
Prof Rob Andrews, Associate Professor, University of Exeter and Honorary Consultant Physician, University of Exeter and Manyee Li, Specialist Dietitian (Diabetes/Sport & Exercise Medicine) Queen Elizabeth Hospital (University Hospitals Birmingham NHS Foundation Trust) will discuss the following therapies: exercise, diet, insulin (all modalities), glucose monitoring
|
|
|
1d - Dealing with multisports
Anne-Marie Frohock, Lead Paediatric Diabetes Dietitian, Oxford University Hospitals NHS Foundation Trust will discuss the following therapies: diet and insulin (MDI, Pumps) and close loop system
|
|
|
1e - Getting the most out of a continuous glucose monitor when exercising
John Pemberton, Diabetes Dietitian, Birmingham Women's and Children's Hospital NHS Foundation Trust and Dr Alistair Lumb, Consultant in Diabetes and Acute General Medicine, OCDEM, Oxford University Hospitals NHS Foundation Trust will cover all types of continuous glucose monitors
|
|
| 11:45 |
Workshops 1a – 1e
|
| Choose your second morning workshop from the following: | |
|
1a - Assessment and starting advice for exercise
|
|
|
1b - Basic insulin changes to improve glucose control around exercise
|
|
|
1c - Special circumstances
|
|
|
1d - Dealing with multisports
|
|
|
1e - Getting the most out of a continuous glucose monitor when exercising
|
|
| 12:35 |
Lunch and networking break
|
| 1:30 |
Exercise setting for each pump / closed loop system and how to use these settings for exercise
In groups attendees will be introduced to each Pump / closed loop system and be talked through features for exercise and how to use. At the end you will receive a summary sheet of the pros and cons of each system and recommendations for which system might suit different people
|
| 2:45 |
Workshops 2a-2e
These workshops will be run twice in the afternoon.
|
| Choose your first afternoon workshop from the following: | |
|
2a - Using dietary intake to improve glucose control around exercise
Claire Foster, Diabetes Dietitian, Somerset NHS Foundation Trust and Manyee Li, Specialist Dietitian (Diabetes/Sport & Exercise Medicine) Queen Elizabeth Hospital (University Hospitals Birmingham NHS Foundation Trust)
|
|
|
2b - Using exercise to control glucose around exercise
Prof Parth Narendran, Diabetes Research Unit and the Type 1 Diabetes Clinical Service Lead, University of Birmingham and The Queen Elizabeth Hospital and Barbara Hudson, Clinical Nurse Specialist in Diabetes, University Hospital Birmingham NHS Foundation Trust
|
|
|
*Recommended for first time attendees*
If this is your first time attending EXTOD day then we would suggest picking the above workshops as these will give you a good grounding
|
|
|
2c - Managing race /event day
Prof Rob Andrews, Associate Professor, University of Exeter and Honorary Consultant Physician, University of Exeter and Giorgio Carrieri, Lead Nurse, Children's Diabetes Team, Somerset NHS Foundation Trust will discuss the following therapies: psychological approaches, exercise (training), diet, Insulin (all modalities), glucose
|
|
|
2d - Dealing with multisports
Anne-Marie Frohock, Lead Paediatric Diabetes Dietitian, Oxford University Hospitals NHS Foundation Trust will discuss the following therapies: diet and insulin (MDI, Pumps) and close loop system
|
|
|
2e - Getting the most out of a continuous glucose monitor when exercising
John Pemberton, Diabetes Dietitian, Birmingham Women's and Children's Hospital NHS Foundation Trust and Dr Alistair Lumb, Consultant in Diabetes and Acute General Medicine, OCDEM, Oxford University Hospitals NHS Foundation Trust will discuss all types of continuous glucose monitors
|
|
| 3:35 |
Networking break
|
| 3:50 |
Workshops 2a – 2e
|
| Choose your second afternoon workshop from the following: | |
|
2a - Using dietary intake to improve glucose control around exercise
|
|
|
2b - Using exercise to control glucose around exercise
|
|
|
2c - Managing race /event day
|
|
|
2d - Dealing with multisports
|
|
|
2e - Getting the most out of a continuous glucose monitor when exercising
|
|
| 4:40 |
Pulling it all together
Prof Rob Andrews, Associate Professor, University of Exeter and Honorary Consultant Physician, University of Exeter will discuss the following therapies: exercise, diet, finger and continuous glucose monitors, insulin, insulin pumps and closed loop systems
|
| 5:20 |
Close of day
|
|
Today’s sponsor, Novo Nordisk, has sponsored a stand space and has had no editorial input into the agenda, content development or choice if speakers.
|
|
EXTOD faculty
Evidence based content delivered by members of the EXTOD faculty, plus additional speakers who are all experts in T1D and exercise:

Giorgio Carrieri
Lead Nurse, Children's Diabetes Team
Somerset NHS Foundation Trust

Dr Matt Cocks
Exercise Physiology Lecturer
Liverpool John Moores University

Claire Foster
Diabetes Dietitian
Somerset NHS Foundation Trust

Barbara Hudson
Clinical Nurse Specialist in Diabetes
University Hospital Birmingham NHS Foundation Trust

Mr John Pemberton
Diabetes Dietitian
Birmingham Women's and Children's Hospital NHS Foundation Trust

Wendy Frost
Lead Dietitian and Leader
Wessex Children and Young People’s Diabetes Network and Team Type One Style
Henry Aspden
Team Type One Style
Past attendee feedback
EXTOD National Conference has taken place since 2017, providing attendees with knowledge, inspiration, and a practical understanding of how to support their Type 1 patients to undertake safe and effective exercise. Over 1,200 people have benefited from this unique education to-date, and here are just a few quotes from their experience at the 2023 and 2024 conferences held in Oxford and Bristol:
Upcoming events
These events are delivered by EXTOD, organised by SBK Events with full details available to view on the Diabetes National Networking Forums website.
EXTOD Sports Coach & PE Teacher Online Training – half day
Thursday 26th September 2024, Engineers’ House, Bristol
This half day online course will arm physical education teachers, or coaches with the tools and techniques required to help children or young people in their care to manage glucose around exercise.
EXTOD Healthcare Professionals South Conference
Friday 6th September 2024, Engineers’ House, Bristol
This new, one day forum is created to equip Diabetologists, Diabetes Specialist Nurses, Dietitians and Paediatricians with the knowledge, inspiration, and practical understanding to support T1D patients who exercise.
EXTOD Adults with Type 1 Diabetes Conference
Saturday 7th September, Engineers’ House, Bristol
Providing interactive tools, clinical cases, shared learning and problem/solution-based tasks, this training day will support adults with diabetes who find exercise challenging.
EXTOD Healthcare Professionals National Conference
Tuesday 26th and Wednesday 27th November 2024, Radisson Blu Hotel, Edinburgh
Featuring evidence-based presentations, case study led workshops and invaluable lived experience of diabetes and exercise.
EXTOD Football Coaches Guide to Supporting Players with Type 1 Diabetes
Wednesday 6th November 2024, Online via Zoom
Created to equip Sports Coaches with the knowledge, inspiration, and practical understanding of how to support type 1 diabetes players to undertake safe and effective exercise.
Sponsored by
Why sponsor?
Our role at SBK Events is to bring industry together with healthcare professionals so that you can educate and inform your audience. These trail-blazing diabetes delivery forums offer dedicated presentations, Q&A, networking and discussion time, each sponsor will be fully immersed into the event and able to effectively engage with your NHS audience.
Interested in having your own event, managed by us?
SBK Events also provides in-house forums. Working closely with you as the client we can research, produce, market and deliver the conference or online forum that best suits the audience and meets your goals.
Reach out today
If you would like more information on our sponsorship options an in-house forum or if you wish to discuss your needs and what solutions may be appropriate for your business, please contact:
Sarah Kemm
Contact: 01732 897788
Email: sarah.kemm@sbk-events.co.uk
Supported by JDRF and the Diabetes Research and Wellness Foundation

DRWF was established in 1998 to raise awareness of all types of diabetes and associated complications. We provide information and support to enhance good self-management, whilst funding vital research to establish the causes, prevention and treatments of Type 1 and Type 2 Diabetes to facilitate diabetes management. We aim to ensure that they are "staying well until a cure is found..."
%20resized.png)
JDRF, the leading global type 1 diabetes charity, works every day to help people live better with the condition, prevent people ever developing it and one day, find cures.
Regular physical activity (PA) plays a key role in the management of Type 1 diabetes mellitus (T1D).
This has been known for years as on the Joslin Victory Medal it is one of the three horses that controls Type 1 diabetes, the other being Insulin and diet.
Figure 1: Joslin Victory medal for living with T1DM
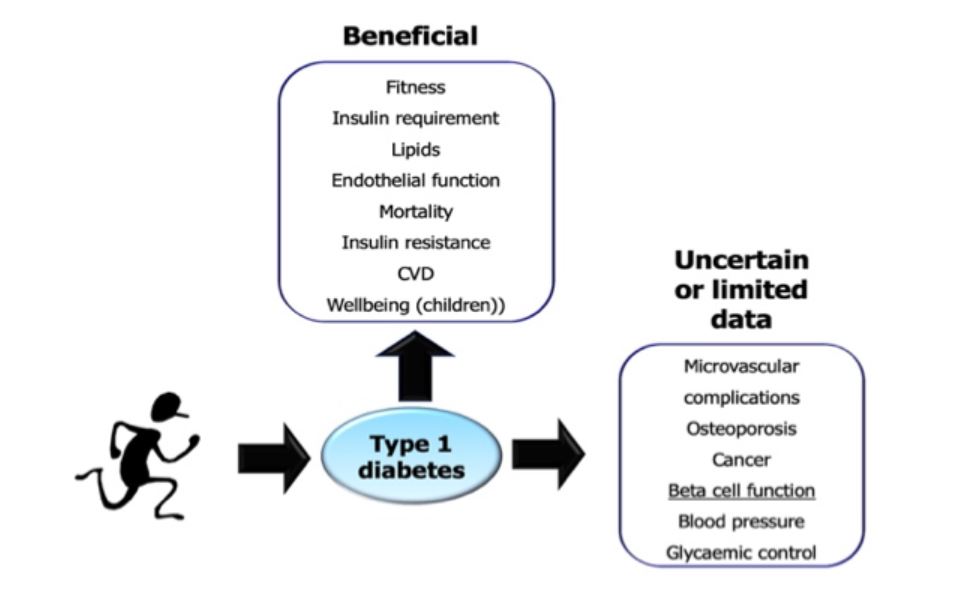
Figure 2 summaries what is known about the benefits of exercise in people with T1D . The known benefits include
- improved insulin sensitivity
- improved well-being
- reduction in lipids
- reduction in microvascular complications
- reduced mortality
For further information see What are the health benefits of physical activity in type 1 diabetes mellitus? A literature review
Figure 2: Summary of health benefits of regular exercise in Type 1 diabetes.
Although there is as yet not conclusive evidence that regular exercise helps to preserve beta cell function there is some evidence to support this
In mice susceptible to diabetes (NOD mouse) regular exercise prevents the development of diabetes. See Exercise Training but not Curcumin Supplementation Decreases Immune Cell Infiltration in the Pancreatic Islets of a Genetically Susceptible Model of Type 1 Diabetes
The Type 1 diabetes honeymoon period is more than five times longer in men undertaking high levels of physical exercise, compared with age‐, sex‐ and BMI‐matched sedentary controls. See The Type 1 diabetes ‘honeymoon’ period is five times longer in men who exercise: a case–control study
In a pilot RCT of newly diagnosed patients with Type 1 diabetes there is some suggestion that exercise preserves beta cell function. See Exercise to preserve β‐cell function in recent‐onset Type 1 diabetes mellitus (EXTOD) – a randomized controlled pilot trial
Note that improvement in HbA1c is not listed as one of the benefits of exercise. A meta-analysis of studies carried out in 2013 by us did not demonstrate an improvement in HbA1c with regular exercise in adults and children with Type 1 diabetes. For more information about this see Does exercise improve glycaemic control in type 1 diabetes? A systematic review and meta-analysis
One reason for this could be that advice given to people with Type 1 diabetes around how to control glucose around exercise is not very good.
Recommended Levels of activity for people with Type 1 diabetes and barriers to exercise
Based on this evidence guidelines recommend that adults with Type 1 diabetes undertake at least 150 min per week of moderate to vigorous aerobic exercise, spread out over at least 3 days, with no more than two consecutive days between bouts of aerobic activity (see Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association and Physical activity levels of people with Type 1 diabetes.
Over 70% of people with Type 1 diabetes do not meet these recommendations and thus are not getting the full benefits they could do from exercise. (See Physical activity levels of people with Type 1 diabetes to learn more about recommended levels of activity for people with Type 1 diabetes and current activity levels of people with Type 1 diabetes.)
Reported barriers to exercise in those with Type 1 diabetes include fear of hypoglycaemia, competing work commitments, loss of control over diabetes, low fitness levels, cost, lack of social support, and lack of knowledge. Greater knowledge about insulin pharmacokinetics and using appropriate approaches to minimise exercise‐induced hypoglycaemia or hyperglycaemia are factors associated with fewer perceived barriers to exercise (see Barriers to exercise in people with Type 1 diabetes to learn more about barriers in Type 1 diabetes).This suggests that the provision of knowledge and skills is essential if we are to support people with Type 1 diabetes to become more active and enable them to exercise safely at the level they wish to.
Other parts of the website should help you to arm your patients with knowledge to overcome these barriers.
Articles linked to this article
Assessment of the patient
People with Type 1 diabetes tend to have four main problems when exercising these are;
- problems controlling their blood glucose during and immediately following exercise
- unexplained severe hypoglycaemia particularly at night
- reduced performance due to excessive fatigue and reduced muscle strength.
- difficulties gain or losing weight
It is important that a detailed history and examination is undertaken to deal with these issues.
Key things in History and examination
Current approaches to managing T1DM
- Patients need to check their glucose regularly when exercising
- Patients who carbohydrate count and use carb/insulin ratios have more options to manage their exercise.
- High blood glucoses – make it difficult to build up muscle mass and glycogen stores post exercise so ideally HbA1c should be a good as possible.
Insulin regime
- It is difficult to manage patients who are performing regular exercise on premixed twice-daily regimes without incurring the risk of exercise-induced hypoglycaemia.
- Fast-acting insulin analogues (Insulin aspart (Novo Nordisk), lispro (Eli Lilly) or glulisine (Sanofi-Aventis)) have a shorter window of action than human, pork or beef insulin which can be helpful if exercising around meal times.
- The longer duration of action of the long-acting basal insulins whilst helpful in routine clinical care, can result in higher insulin concentrations during exercise and an increased risk for hypoglycaemia during endurance exercise and less flexibility in reducing dose post exercise
- In one clinical study NPH insulin (insulatard (Novo Nordisk), Humulin I (Eli Lilly)) and determir (Novo Nordisk) had lower risk of hypoglycaemia with exercise than glargine (sanofi-aventis)(see Plasma glucose and hypoglycaemia following exercise in people with Type 1 diabetes: a comparison of three basal insulins.)
- In another study glargine had similar rate of hypoglycaemia after exercise as Degludec (Novo Nordisk). (see Similar risk of exercise‐related hypoglycaemia for insulin degludec to that for insulin glargine in patients with type 1 diabetes: a randomized cross‐over trial).
- No studies to data have looked at Insulin glargine u300 (Toujeo – Sanofi-aventis) or Abasaglar (Biosimilar Glargine – lilly) and exercise in Type 1 diabetes.
- Changes to insulin rates and background rates during and post exercise can be different to those on MDI regimes (see Pumps and exercise).
Insulin injection techniques
- The aim to reduce day-to-day variation in insulin absorption and to avoid accelerated absorption of insulin when exercising.
- Injection sites should be checked to ensure there is no lipohypertropy.
- Injection techniques should be checked to ensure that air shots are being given. If the patient is on NPH insulin resuspension should be carried out correctly.
- Needle sizes should also be checked - 4 or 5mm needles are to be recommended.
- Patients should also be educated to avoid injecting into areas that will be used in planned exercise (eg. thighs before cycling) because the increased blood flow will increase insulin absorption.
Diabetes complications
- For most people with T1DM any activity can be undertaken and risk is minimal if people start at a low intensity of activity and gradually build up the intensity.
- Some diabetes complications restrict what people with T1DM, others suggest that further investigations should be done before exercise is started (see Exercise and microvascular complications and Exercise and macrovascular complications).
- Feet will need to be examined to look for: ulceration, deformity and evidence of neuropathy.
- Eye report/photos should be looked at so assess whether the patient has retinopathy if so what level.
Review of calorie intake
- Ensuring adequate fuel and fluid replacements is one of the most important components in ensuring safe and effective training in people with Type 1 diabetes.
- A common cause of hypoglycaemia and of fatigue during and following exercise is simply one of insufficient calorie intake.
- For these reason, all patients should have their dietary intake assessed if doing more than 1 hour a day of moderate intensity exercise. Ideal this should be done by a dietician.
A detailed history of exercise program
- The type, duration and intensity of exercise will determine blood glucose fluxes both during and after exercise. Endurance events will tend to lower glucose (see Types of exercise and their effects on blood glucose.)
- Anaerobic or intense exercise will tend to increase glucose during and on occasions after exercise (See Types of exercise and their effects on blood glucose).
- This knowledge will influence the advice provided on what to do with starting glucoses (see Blood glucose and exercise for adults with T1D).
- Similarly, this knowledge may influence the advice given on carbohydrate intake (Carbohydrates for exercise for people on multiple daily injections and Carbohydrate for exercise for people on insulin pumps) and insulin therapy.
History of performance in training and competition
- The approach to glucose management (for example the starting blood glucose) may need to be different in training and competitive events (seeBlood glucose and exercise for adults with T1D).
- Exploring performance in these two settings will enable the optimal approach to be designed for each of these settings
Articles linked to this article
Exercise and microvascular complications
Exercise and macrovascular complications
Fuel and fluid for exercise
Types of exercise and their effects on blood glucose
Blood glucose and exercise for adults with T1D
Carbohydrates for exercise for people on multiple daily injections
Carbohydrate for exercise for people on insulin pumps
In simple terms there are
three ways that glucose can be managed during exercise. The easy way to
remember these is through the mnemonic ‘ICE’.
I Insulin adjustment
C Carbohydrate for exercise
E Exercise - changing type or intensity
Insulin adjustment for exercise
The
liver is main source for carbohydrate that is used when exercising.
When insulin levels are high, the liver is prevented from releasing
glucose (see glucose control during exercise). High insulin levels
during exercise could therefore lead to a mismatch between the glucose
produced by the liver and that used by the muscles. This will result in a
fall in circulating blood glucose falling during exercise.
Ideally
patients should exercise with as little insulin around as possible.
Changes can be made to the quick-acting (bolus) or the background
(basal) insulin to help with this. What changes are made to insulin will
depend on the type, intensity and length of the exercise and on what
time of day the exercise is carried out.
Carbohydrate for exercise
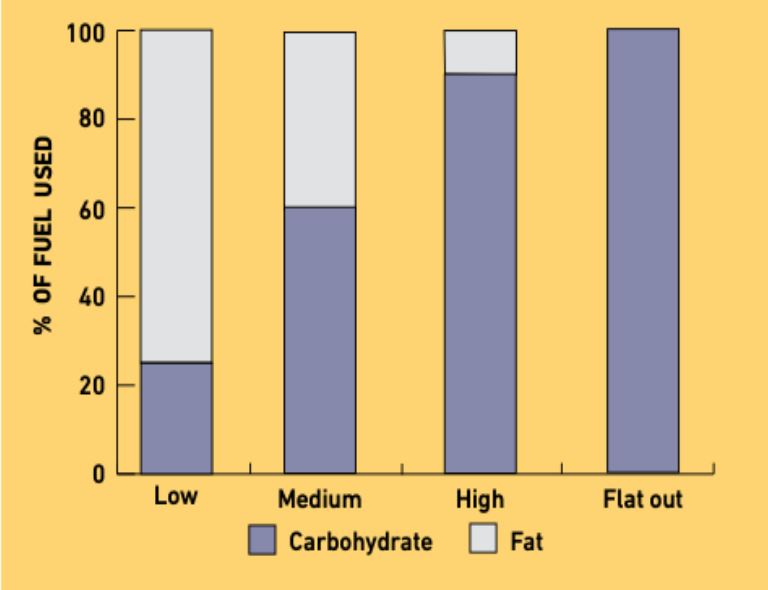
The
two main fuels used during exercise are fats and carbohydrates (in the
form of glucose). People with Type 1 Diabetes burn fat normally during
exercise; it is only the production of carbohydrate that they have
problems with.
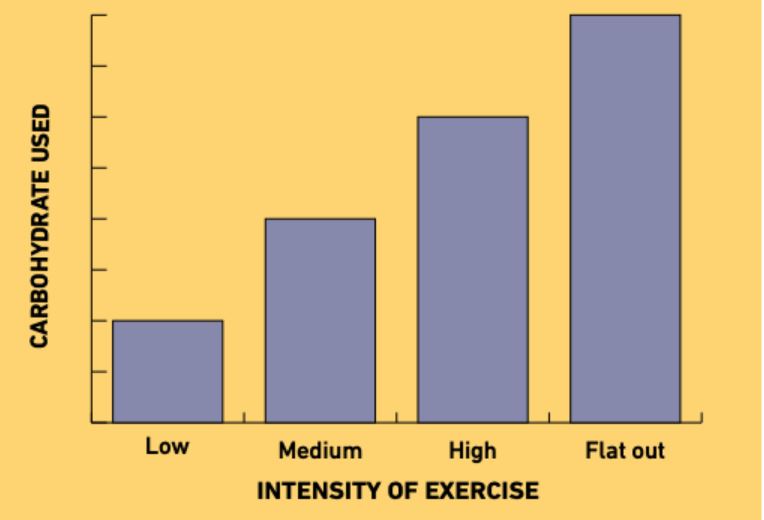
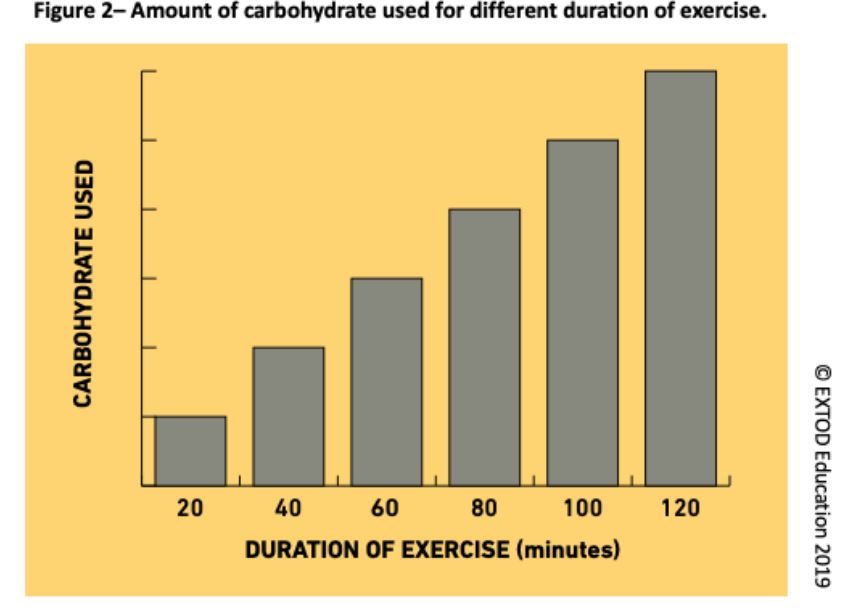
The exercise carbohydrate value of an exercise is the
amount of carbohydrate that is used during an exercise. The higher the
exercise’s intensity, the more carbohydrate is burned per minute see
figure 1 below.
The amount of carbohydrate needed will also depend on the age, sex, weight and fitness of the person performing the exercise.
When
using carbohydrates for exercise, the aim is to take all the
carbohydrate needed to perform the particular exercise so that the
glucose remains stable across the exercise.
To find out more, go to Carbohydrates for exercise for people on multiple daily injections.
Exercise adjustment for exercise
Different exercise regimes have different effects on blood glucose concentration (see Types of exercise and their effects on blood glucose).
This knowledge can be used to help control glucose during exercise.
Changing the order in which exercise is done or adding a different type
of exercise can help with glucose control during exercise.
To find out more about this go to exercise adjustments for exercise.
Summary
Each of these strategies has its pros and cons. The table below is a summary of the pros and cons. This may be helpful in deciding which strategy you choose to recommend first to your patients
Strategy | Pros | Cons |
Insulin adjustment for exercise | Reduces hypoglycaemia during and following exercise, reduces carbohydrate requirement | Needs planning. Not helpful for spontaneous exercise. Changing bolus insulin dose is not helpful if exercising 2 hours outside the bolus. |
Carbohydrate for exercise | Useful for unplanned exercise | May not be possible with some exercises. Not helpful where weight control important. May over-replace so blood glucose goes too high. |
Exercise adjustment for exercise | Useful for unplanned exercise | May not be possible with some exercises. May not always have desired effect, lowering glucose or raising glucose more than needed. |
Definition of exercise
Physical activity is defined as any bodily movement produced by skeletal muscles that results in energy expenditure. Physical activity in daily life can be categorized into occupational, sports, conditioning, household, or other activities. Exercise is a subset of physical activity that is planned, structured, and repetitive and has as a final or an intermediate objective the improvement or maintenance of physical fitness.
Exercise is performed for various reasons, to aid growth and improve strength, preventing aging, developing muscles and the cardiovascular system, honing athletic skills, weight loss or maintenance, improving health and also for enjoyment. For more details on the health benefits of exercise for people with Type 1 diabetes.
Guidelines recommend that adults with Type 1 diabetes undertake at least 150 min per week of moderate to vigorous aerobic exercise, spread out over at least 3 days, with no more than two consecutive days between bouts of aerobic activity. In addition, muscle-strengthening activities that involve all major muscle groups should be performed on two or more days per week. For more information on recommended levels of activity for people with Type 1 diabetes see Physical activity levels of people with Type 1 diabetes section of this website
Being able to define what type of exercise what type of exercise a patient does is key to understanding what will happen to their blood glucose when they perform that exercise. This will also help you to work out how much energy the patient will burn during that exercise and any changes you may need to suggest to their insulin regimen and eating patterns when performing that exercise.
The Pyramid of fitness
In simple terms, to improve at any type of exercise you need to work on four areas (see figure 1).
Figure 1 - the pyramid of fitness
How much someone needs to work on each of these will depend on what exercise they are doing.
Defining a patient’s exercise
Defining exactly what a patients does should form part of the initial assessment of a patient (see Initial medical assessment of patient with Type 1 diabetes in relation to exercise part of this website.
To give good tailored advice to a patient you will need to know determine three things:
- What type of activity the patient is doing (click here to learn more about this)
- How intense the activity is (click here to learn more about this)
- How long the activity will last for (click here to learn more about this)
Once you have learned this you are ready to start to give advice on how your patient can manage glucose around exercise (see Encouraging patients to exercise and starting advice section of this website).
How much someone needs to work on each of these will depend on what exercise they are doing.
Defining a patient’s exercise
Defining exactly what a patients does should form part of the initial assessment of a patient (see Initial medical assessment of patient with Type 1 diabetes in relation to exercise part of this website.
To give good tailored advice to a patient you will need to know determine three things:
- What type of activity the patient is doing (click here to learn more about this)
- How intense the activity is (click here to learn more about this)
- How long the activity will last for (click here to learn more about this)
Once you have learned this you are ready to start to give advice on how your patient can manage glucose around exercise (see Encouraging patients to exercise and starting advice section of this website).
Defining a patient’s exercise
Defining exactly what a patients does should form part of the initial assessment of a patient (see Initial medical assessment of patient with Type 1 diabetes in relation to exercise part of this website.
To give good tailored advice to a patient you will need to know determine three things:
- What type of activity the patient is doing (click here to learn more about this)
- How intense the activity is (click here to learn more about this)
- How long the activity will last for (click here to learn more about this)
Once you have learned this you are ready to start to give advice on how your patient can manage glucose around exercise (see Encouraging patients to exercise and starting advice).
Recommended levels of activity
Shown below is the recommended levels of activity for adult, children and pregnant women with Type 1 diabetes.
| Adults |
|
Children |
|
| Pregnancy |
|
How active are people with Type 1 DM
Most
studies of physical activity (PA) levels in adults with Type 1 diabetes
have been based on self-reported data rather than objective data. They
all suggest that people with Type 1 diabetes are not very active.
Self-reported studies
- A retrospective analysis of the Diabetes and Complications Trial found 19% of (271/1441) participants were not achieving recommended PA levels (see - Effects of physical activity on the development and progression of microvascular complications in type 1 diabetes: retrospective analysis of the DCCT study).
- In the EURODIAB prospective cohort study of 2185 people with Type 1 diabetes from 16 European countries, 786 (36%) patients were doing no or only mild PA (see - Association of physical activity with all-cause mortality and incident and prevalent cardiovascular disease among patients with type 1 diabetes: the EURODIAB Prospective Complications Study).
- In the Finnish Diabetic Nephropathy Study, 23% of people with Type 1 diabetes were classed as sedentary and a further 21% were doing less than one session of exercise per week. (see - Physical Activity and Diabetes Complications in Patients With Type 1 Diabetes. The Finnish Diabetic Nephropathy (FinnDiane) Study).
- In a cross sectional study of 18028 patients with Type 1 diabetes in Germany and Austria 63% of participants reported doing no regular PA (see - Impact of Physical Activity on Glycemic Control and Prevalence of Cardiovascular Risk Factors in Adults With Type 1 Diabetes: A Cross-sectional Multicenter Study of 18,028 Patients).
Objectively measured PA
- In a Canadian study of adults with Type 1 diabetes only 43% of women and 55% of men with Type 1 diabetes were active (see - Physical activity level and body composition among adults with Type 1 diabetes).
- In a UK study of adults with Type 1 diabetes, adults with Type 1 diabetes undertook 37 mins per day of moderate to vigorous physical activity compared to 52.9 mins per day in healthy matched controls. (see - Objective Measurement of Physical Activity in Adults With Newly Diagnosed Type 1 Diabetes and Healthy Individuals).
The
reasons for the reduced level of physical activity could be due to that
additional barriers that people with Type 1 diabetes have to physical
activity.
Patients with Type 1 diabetes have many barriers to exercise that are similar to the general populations such as
- Lack of time
- Work pressures
- Bad weather
- Cost
- Lack of motivation
But there are certain barriers that are specific to them, see table below.
Table showing barriers to physical activity in patients with Type 1 diabetes.
| New onset Type 1 diabetes | Established Type 1 diabetes |
|
|
To be able to increase activity these barriers will have to be overcome.
For more information on this subject see
- Brazeau A.S et al paper (Barriers to Physical Activity Among Patients With Type 1 Diabetes. Diabetes Care. 2008;31(11):2108-9).
- Dubé MC et al paper (Development and validation of a new scale. Diabetes Research and Clinical Practice. 2006;72(1):20-7).
- Lascar N et al paper (Attitudes and Barriers to Exercise in Adults with Type 1 Diabetes (T1DM) and How Best to Address Them: A Qualitative Study).
- Kennedy A et al paper (Attitudes and barriers to exercise in adults with a recent diagnosis of type 1 diabetes: a qualitative study of participants in the Exercise for Type 1 Diabetes (EXTOD) study).
Please login to access documentation associated with the event. This is an exclusive benefit for all of the attendees and includes additional and updated documentation.